Get Started with Above Diabetes
Whether you’re a patient or a clinic looking to expand your offering, we’re here for you.

For Patients
Ready to achieve better diabetes management? Click below to learn more if Above Diabetes is the right fit for you and your diabetes needs.

For Clinics
Are you a clinic without diabetes specialist? Partner with Above Diabetes for essential adjunct support in patient education.
We collaborate with clinics & pump providers:





PARTNERSHIP SERVICES
We collaborate with your clinic to deliver clinical trial services, we offer expert dietary counseling, diabetes education, and top-tier pump training and follow-up services to your patients.
CLINICAL SERVICES FOR RESEARCH PARTICIPATION
Enhancing your practice’s engagement in clinical trials with expert dietary counseling and comprehensive diabetes education services, fostering research and innovation in patient care.
* Good Clinical Practice (GCP) Certified

CERTIFIED PUMP TRAININGS & QUALITY SUPPORT
Our team, comprised of experienced educators living with T1D, collectively offers over 60 years of pump experience. We are dedicated to enhancing your clinic’s services by providing expert certified pump training and follow-up.
SUPPORTED PUMPS: Tslim X2 & Mobi with Tandem, 780G with Medtronic, Dash & Omnipod 5 with Insulet, iLet with Beta Bionics

DIETARY COUNSELING & DIABETES EDUCATION
We specialize in dietary counsel and diabetes education. With in-network coverage and Medicare, we also offer discounts for out-of-network patients, along with Spanish-language classes. Our services come with streamlined billing and claims management.
Meet our Amazing health professionals
Above Diabetes educators are dedicated healthcare professionals specialized in tailored diabetes care; empowering you to thrive with your diabetes.
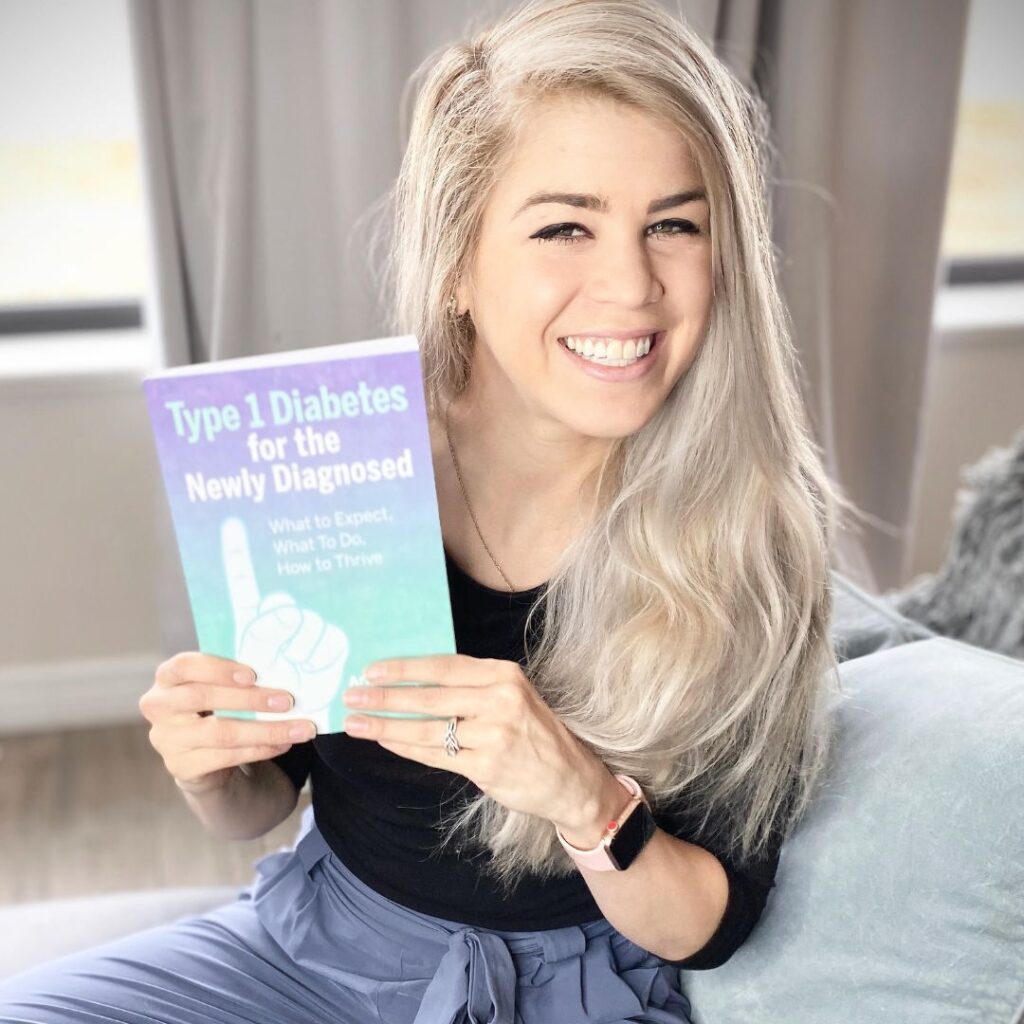
Ariel Warren
RDN, LD, CDCES
Utah & Texas Availability
Diagnosed in 1995, she is experienced with all FDA-approved pumps and lifestyle behavior modification to help people with diabetes reduce medication and total insulin usage and to improve quality of life.
* Multi-time published author in diabetes education and recipe books.

AnneMarie Rousseau
DNP, FNP-BC, APRN, CDCES
Utah Availability
Diagnosed with type 1 in 2000; AnneMarie is an experienced Family Nurse Practitioner specializing in all types of diabetes, with a special interest in gestational care for mothers with diabetes.
* Awarded ‘Diabetes Educator of the Year’ by ADCES Utah in 2022.

Annette Valle
RN, BSN, CDCES
Utah Availability
Diagnosed with type 1 in 2000; Annette is a Registered Nurse who has over a decade of experience. Annette enjoys working with people with exercise strategies and helping patients live their best life with diabetes.
* Fluent in Spanish
ACCREDITED BY ADCES:
We are proud to be an accredited Diabetes Self-Management Education and Support (DSMES) program by the Association of Diabetes Care & Education Specialists (ADCES). This accreditation ensures that our program meets the highest standards of quality and effectiveness in diabetes education.
See what people are saying.
Our happy patients have a lot to say about our education!
9.0% to 6.0% in 6 Months
”I decided to make a virtual appointment with Ariel because my blood sugars were really out of control. I can honestly saw that Ariel and her diabetic education program have changed my life! My blood sugars have never been better. My A1c has come down from 9.0 to 6.0% in just 6 months! She is so encouraging, so professional, and so knowledgable about EVERYTHING diabetes-related. Overall an amazing person with the BEST program for people with type 1 diabetes.”

Shelly
T1DNewly Diagnosed with Type 1
“I was diagnosed with Type 1 Diabetes in 2017 and from the beginning I was determined to stay healthy but despite my efforts I struggled to manage my blood sugar. Ariel has done an incredible job in helping me to understand T1D and how diet and exercise affect my blood glucose levels. She’s taught me how to use my insulin pump much more effectively and with her help I have been able to maintain a lower A1C.”

Karli
Author6.3% to 5.2% in 3 Months
“Working with Ariel has finally given me the experience of relating to another Type 1 with similar goals as mine that I have always been searching for! Working with her has helped me grow independently with my diabetes care! She helps make the day to day stress of living with Type 1 Diabetes somewhat less stressful! I am so thankful to be working with her! :)”

Natalie
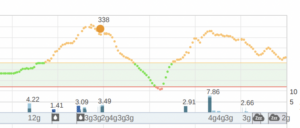
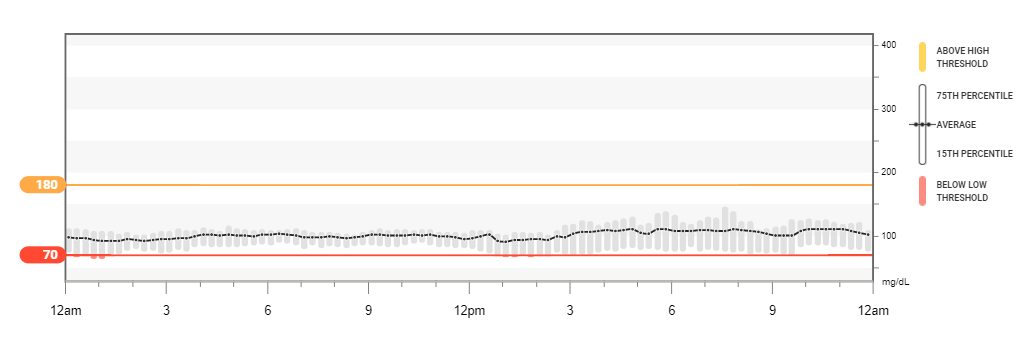
T1D100% Time in Range for 7 Days
“I started working with Ariel when I switched to the T-Slim X2 pump with Control IQ. Working together has become the highlight of my week. Together, we work on getting my profiles accurate (basals, carb ratios, correction factors), and we work on my nutrition, exercise, stress, sick days, my COVID19 fears, traveling, and any other personal struggles. Ariel has an amazing work ethic and overall goal to make your diabetes management less of a burden so it leaves you more freedom to live your life. She is now a personal friend.”

Paula
T1D8.2% to 6.4% in 3 Months
“Before beginning to work with Ariel Warren, my previous HA1c results were 8.2 and higher. After just 3 months of weekly coaching I am proud to say that my latest HA1c came in at 6.4!
Ariel makes available a unique and curated set of skills to her clients. She is professionally certified, understands the science and is a high personal achiever…yet she is somehow able to adapt to the specific needs of her client, gently meet them where they are, and invite them into a series of attainable personal victories and greater health.”
Brad
T1.5DLost 52 lbs & My HbA1c Down to 5.5%
“Today, after 4 months working Ariel, I’m down 52 lbs, I’ve reversed my diabetes. My doctor not only took me off the diabetic list, but even the pre-diabetic list! I don’t take any metformin and I sit at a 5.5% A1c.”

Lynn
T2DCommonly Asked Questions

What services does Above Diabetes provide?
- Pump Success Program: Comprehensive training package covering pre-training, pump selection, certified training, and personalized post-training support.
- Advanced Insulin Intensive Therapy & Data Analysis: Optimizing settings through data analysis with the patient to empower patient with changes.
- ADCES Self-Care Behaviors Integration: Empowering sustainable lifestyle changes through motivational interviewing.
- Pregnancy & Diabetes Care: Specialized support for expectant mothers with diabetes.
- Stress, Sickness, & Lifestyle Adjustments: Coping strategies for managing challenges.
- Strategic Exercise Planning & Insulin Dosing: Tailor insulin dosing for various exercise types, timings, and meal planning to stabilize blood sugar.
- Sick Days & DKA Prevention: Expert guidance during illness to prevent diabetic ketoacidosis.
- Precise Meal Dosing & Advanced Bolusing: Mastering mealtime insulin dosing and advanced bolusing techniques.
- Remote Monitoring: Fine-tuning pump settings from a distance for optimal control.
How do I get started/get a patient started?
For commercial, please send a referral and the most recent chart note and labs.
Fax Number: 801-702-8143
Which Insurances are Accepted?
Utah: we currently accept Regence, Aetna, UHC, PEHP, and Select Health
Texas: we currently accept, BCBS, BSW (tier 2), Aetna, and UHC
If you do not have insurance, we have discounted cash-pay options and further discounted group classes.
Do you meet in-person?
While Above Diabetes is mostly virtual for Texas and Utah, we are able to meet patients or doctors at clinics near our physical residences.
Are you ready for improved diabetes management?
Committed educators in Utah and Texas, facilitating self-discovery, solutions, and behavior change. Covered by most commercial insurances and Medicare.
Diabetes Education Articles
Highly Processed Dairy and Insulin Resistance: A Comprehensive Guide for People with Diabetes
Discover the complex relationship between highly processed dairy, insulin resistance, and weight loss. Explore how dietary choices can impact diabetes control and gain insights into making informed nutritional decisions. Also learn the differences in saturated fat coming from highly processed dairy and grass-fed meats.
Low Cost & Quality Dietary Counsel Through Insurance in Utah & Texas: Weight Loss, Diabetes, PCOS, and Insulin Resistance
Embark on a journey to optimal health with free dietary counseling from a skilled dietitian in Utah and Texas. Specializing in diabetes, PCOS, and insulin resistance, our expert offers tailored guidance, over 100 recipes, personalized workout programs, and more. Transform your lifestyle and manage health conditions effectively.
Revolutionizing Health: Supercharging Type 2 Diabetes Management with Intermittent Fasting
This powerful lifestyle intervention offers a fresh and exciting perspective, igniting hope for millions of individuals living with type 2 diabetes.